AMD Therapies on the Horizon
Researchers are taking a hard look at new treatments for macula reconstruction.
BY LOUISE GAGNON
More than 11 million Americans have some form of macular disease, according to American Health Assistance Foundation estimates. Because that number is expected to double by 2050, investigators and life science companies have poured considerable resources into finding new sight-preserving treatments.
These treatments include regenerative medications, translocation surgery, transplantation of the RPE, human embryonic stem cells and complimentary therapies. This article provides a cursory view of these emerging treatments, featuring comments from the third University of Toronto, Walter Wright Ophthalmology Conference.
Regenerative Medicines
For many AMD patients, vision is now salvageable thanks to advances in retina care. As far as those advances in retina treatment options go, much of the focus has been on anti-VEGF therapies and photodynamic therapy (PDT). However, despite the efficacy of these treatments, anti-VEGF therapies are not perfect. They fail to provide substantial regression of disease, leaving an unmet need in terms of restoration of vision.
“Anti-VEGF therapy remains excellent compared to what we had before and is excellent compared to no treatment at all,” says Lyndon da Cruz, MA, PhD, a consultant vitreoretinal surgeon at Moorfields Eye Hospital in London.
Surgeons are aiming to restore vision, possibly to levels before the onset of disease, he says. This next big stride in therapy is what some researchers call regenerative medicine. “Anti-VEGF therapy is palliative,” says Dr. da Cruz, “It never reconstructs the disease and never alters the disease. Ultimately, we would like to be able to reconstruct the macula.”

Figure 1. Intraoperative view of full macular translocation surgery. Studies show promising results for translocation surgery, but the procedure has its risks.
Translocation Surgery
Surgery is not a new treatment for AMD. Robert Machemer, MD, a pioneer in the field, developed translocation surgery in the early 1990s (Figure 1). This clinical development dramatically boosted quality of life for AMD patients who could perform daily activities such as reading and driving that they could not otherwise perform.
“There is a period where you have healthy retina and severe disease,” Dr. da Cruz says. “Leaving that situation alone leads to irreversible vision loss. The concept is to separate the macula from the sub-retinal disease after vision loss, but before there is irreversible retinal damage.”
The outcomes of translocation surgery, according to one study, have shown 25% of these patients were able to maintain a three-line gain in acuity for three years, with close post-operative monitoring and early treatment of delayed complications.1 The success of translocation surgery shows that, by restoring healthy sub-retinal tissue, visual function can be restored, Dr. da Cruz says.
Although translocation surgery has been performed for two decades, its practice is not widespread. Dr. da Cruz attributes this to the extensive nature of the procedure. Complications such as proliferative vitreoretinopathy also act as a disincentive to performing translocation surgery. Other reported side effects include diplopia, hypotony and corneal decompensation.
Evaluating the Outcomes
However, outcomes in pilot research have shown gains in both reading speed and acuity. In Dr. da Cruz’s pilot study, about 70% of patients reached 20/80 or better and 25% achieved to 20/40 or better. Almost half gained three lines of visual acuity.2,3
“Not only did they double their reading speed, but they doubled their reading speed with three lines smaller print,” Dr. da Cruz says. “If you look at a person with normal AMD, as the size of the print decreases, so does their reading speed. In this study we were able to see, going from preoperative to postoperative, that they returned to normal reading speed. It was a sign we were reconstructing a healthy macula and not palliating something that will die soon.”
Dr. de Cruz’s investigative team also conducted microperimetry tests and found restoration of normal macula function. Those outcomes, however, were limited by the recurrence of disease, particularly in the absence of other treatments, including anti-angiogenic VEGF inhibitors or photodynamic therapy. With the advent of these therapies, the improvements realized with translocation surgery could then be sustained with adjunctive therapies.
Timing the surgery was not a known variable from the outset, but analysis of the data allowed Dr. da Cruz and his colleagues to establish a cut-off for surgery of six weeks from the time of diagnosis. In cases, for example, where the surgery had been conducted at 10 weeks after the diagnosis, patients were shown to have had the same visual acuity after surgery as they did prior to surgery. “We found that the critical time was about six weeks,” he says.
Transplantation for the RPE
Another intervention to treat macular disease is transplantation of the RPE. With either translocation or transplantation, the type, state and severity of AMD are not variables, but the health of the retina is key to the success of surgery.
Dr. da Cruz and colleagues adopted an approach developed by Jan van Meurs using autologous peripheral RPE cells.4 They performed standard sub-macular surgery through a small retinotomy, where patients underwent a full thickness choroidal epithelium-free graft. The investigators demonstrated postoperative reperfusion in many cases, good pigment epithelium structure and function, and normal retinal anatomy and function. The grafts survived and microperimetry revealed evidence of retinal function over perfused and auto-fluorescent grafts.5
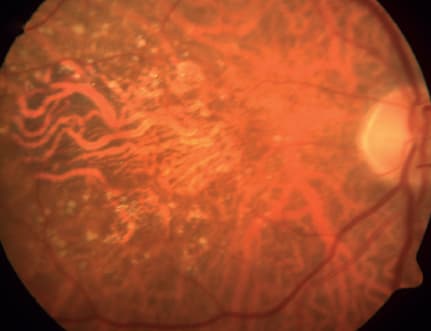
Figure 2. Geographic atrophy in AMD was one of the first targets for clinical trials of pluripotent, stem cell–based therapies. Stem cell therapies are being considered for non-responsive patients to anti-VEGF treatments.
However, they documented a loss of visual acuity and reading ability. Translocation, in comparison, was found to be a more predictable procedure and more effective in improving visual acuity than transplantation.
Dr. da Cruz’s research with transplantation laid the groundwork for further exploration of the technique. “For us, it was proof of principle that if you could put healthy epithelium in a vascularized environment, you could save macular function, and this is something we wanted to chase,” he says. That chase triggered a search for a solid supply of pigment epithelium to respond to untreatable retinal disease.
“We were like looking for something to ‘take out of the fridge,’ just as you would have an intraocular lens ready for cataract surgery,” says Dr. da Cruz. “If you have a cell that can become anything and it can replicate indefinitely, you can have an endless supply of what you want.”
Human Embryonic Stem Cells
Clinicians at Jules Stein Eye Institute at UCLA have successfully transplanted specialized retinal cells derived from human embryonic stem cells (hESCs) in one patient with Stargardt’s disease and another patient with dry AMD. The results were publicized in early 2012. (Figures 2 and 3)
Dr. da Cruz’s team at Moorfields plans to start a therapeutic trial using hESCs. In the short-term, they will treat patients with RPE tears, exposed fovea and massive hemorrhage. Their initial energies will focus on treating patients with wet AMD, as well as those who have not been responsive to VEGF inhibitors.
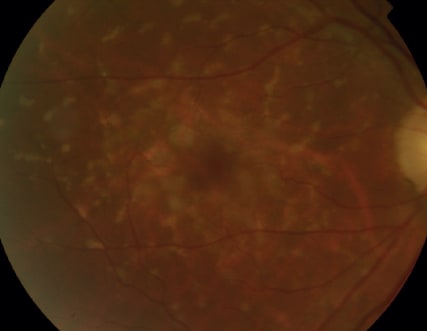
Figure 3. Clinicians have successfully transplanted specialized retinal cells from human embryonic stem cells in a patient with Stargardt’s disease. Stargardt’s disease is shown here using color fundus imaging.
If the short-term outcomes prove successful, Dr. da Cruz and his team will move on to patients with early, non-exudative AMD disease as well as patients who have been on VEGF inhibitors for a number of years and are no longer reaping benefit from the anti-angiogenic agents.
“We will get a good and quick answer as to whether it works, but we are actually developing it for patients with dry AMD,” Dr. da Cruz says. “In the long run, the aim is to reconstruct the macula when it is getting a bit old.”
The concept may sound fanciful, but Dr. da Cruz points out cataract surgery was once a major and often dangerous procedure, but now it’s routine.
Stem cells are more effective than alternatives such as induced pluripotent stem cells, Dr. da Cruz suggests. hESCs “are the ones that are powerful enough to turn over at a rate to produce therapeutic levels of high-quality cells, and they happen to be zero years old,” he says. “The current process with IPS cells is very slow.”
Complementary Therapies
Stem cells, however, probably won’t replace other therapies. Dr. da Cruz says its best to approach the problem from multiple angles.
“They do not have to be competitive,” Dr. da Cruz says. “They can, in fact, be complementary. Treatment can become multi-modal. People start to fail anti-VEGF therapies, and you start to see a decline in function and evidence of combined wet and dry AMD. They may need broader treatment, and that is where we feel we will come in. In the long term, we would hope to combine multiple treatments to manipulate cells and reconstruct the macula.”
If stem-cell transplantation is proven safe and reproducible, ophthalmologists could reconstruct the macula for patients with multiple, soft drusen, he says. It is yet another illustration of regenerative medicine.
The chameleon-like quality of stem cells may also give rise to unwanted tumors, such as teratomas, after transplantation, but some researchers have been looking into avenues that would avoid the formation of these tumors.5 What allays Dr. da Cruz’s fears is that RPE is an endpoint cell that is relatively stable.
Taking the challenges into consideration, Dr. da Cruz envisions a positive outlook for using stem cells in the management of retinal conditions. “The available evidence suggests stem-cell therapies are likely to play a therapeutic role in retinal disease in the near future,” he says. OM
References:
1.Chen FK, Patel PJ, Uppal GS, et al. Long-term outcomes following macular translocation surgery in neovascular age-related macular degeneration. Br J Ophthalmol. 2010;94:1337-1343.
2. Uppal GS, Milliken A, Lee J, et al. New algorithm for assessing patient suitability for macular translocation surgery. Clin Experi Ophthalmol. 2007;35:448-457.
3. van Meurs JC, ter Averst E, Hofland LJ, et al. Autologous peripheral retinal pigment epithelium translocation in patients with subfoveal neovascular membranes. Br J Ophthalmol. 2004;88:110-113.
4. Chen FK, Uppal GS, Rubin GS, et al. Evidence of retinal function using microperimetry following autologous retinal pigment epithelium-choroid graft in macular dystrophy. Inve Ophthalmol Vis Sci. 2008;49:3143-3150.
5. Rong Z, Fu X, Wang M, Xu Y. A scalable approach to prevent teratoma formation of human embryonic stem cells. J Bio Chem. 2012 21:287:32338-32345.
| Louise Gagnon is a freelance medical journalist based in Toronto. |








